Authors: Tiara Askew, Derek Lee, and Kelley Robinson
Mr. C arrived at our emergency department disheveled and lethargic—he smelled of alcohol and his scent permeated the unit.
Nothing but his appearance suggested he was homeless, but without hesitation we labeled him Delta Platinum—just like Delta Airline’s frequent-flyer program. We just knew he would be back again. So the visit was routine and we offered him the bare minimum of care. He was discharged the next morning with a sandwich and a Coke, and he came back the next day.
And the day after that… and the day after that…
Mr. C’s story is not unique. There are an estimated 2,669 people experiencing homelessness in Baltimore city alone, and 6,561 in the entire state of Maryland. People experiencing homelessness (shelter and street) exist in the shadows of society. They are one of the most vulnerable populations in America, and one of the sickest. Nurses take an oath to be a patient’s advocate and closest confidant, but we can still become complicit in perpetuating the discrepancy in the quality of health care delivery and services people experiencing homelessness receive compared to the housed population.
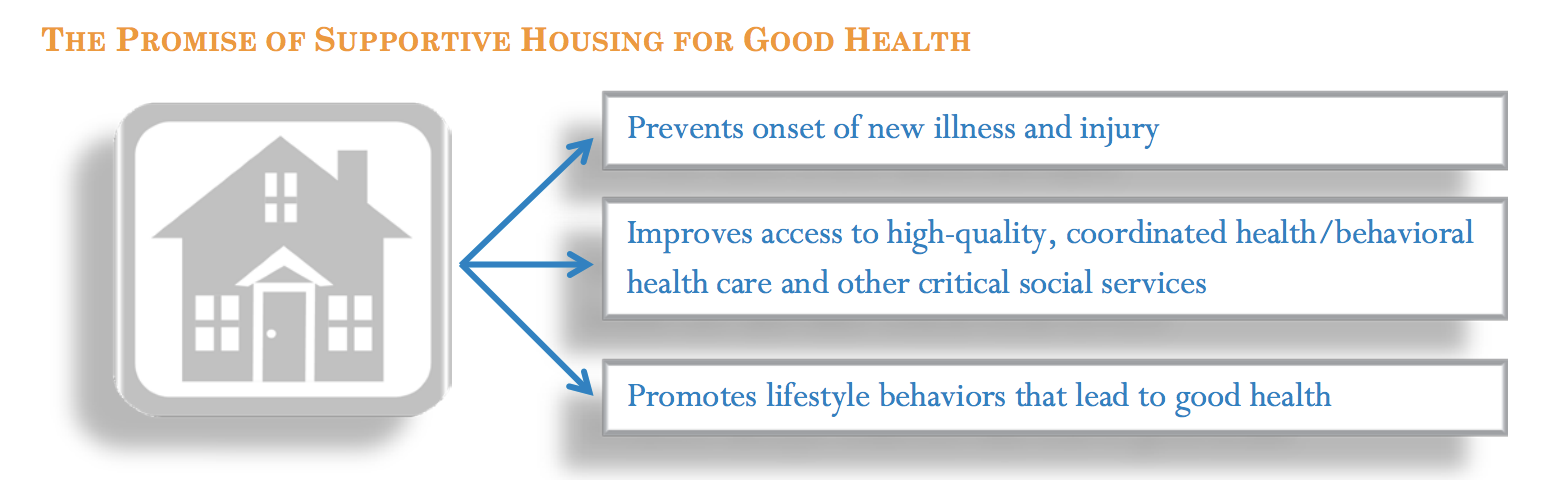
Poor health and homelessness are intertwined.
Poor health is a risk factor for becoming homeless; once homeless, health problems can quickly become worse and new health issues often arise. People experiencing homelessness are diagnosed with chronic health conditions like hypertension, tuberculosis, and depression more often than the general American population. And homelessness and mental illness are related; six percent of the general population suffer from a severe mental illness, but the number rises to upwards of 30 percent among people experiencing homelessness. And more than 50 percent of people who experience homelessness and have a severe mental illness are Black or Latino.
All shareholders involved in the patient’s care can do more to mitigate the challenges faced by this vulnerable population, and nurses are integral to accomplish this goal. While there is no “one-size-fits-all” solution, we can start by building rapport. That’s easier if patients are met on their own turf—shelters, soup kitchens, and on the street.
Mobile Health Clinics (MHCs) are an innovative delivery system for the kind of care that patients typically receive in an outpatient primary care center. Patient outcomes are better and health care is more efficient when patients use primary care to treat chronic physical conditions. It is even more pertinent for individuals with mental health disorders. MHCs can mitigate many of the barriers unhoused patients experience when seeking health care and potentially save upwards of $4 billion annually as a result of decreased emergency department visits. This money could be reinvested into building up a workforce of nurses and nurse practitioners who specialize in community health and psychiatric and mental health to staff MHCs.
Nurse practitioners, in particular, are a high quality, cost-efficient supplement to care for this population. They have significantly decreased the primary care clinician shortage and the profession includes a variety of specialty areas that support people experiencing homelessness, like family nurse practitioners or psychiatric mental health nurse practitioners.
It’s not enough to be credentialed in nursing.
We need to advocate for a restructured nursing curriculum that reflects a higher level of understanding and respect for the social determinants that impact health, so the next generations of nurses are better prepared to treat them.
More importantly, we need to see our biases towards people experiencing homelessness, correct our negative and dismissive language, and provide quality care without judgement. We need to see the “Mr. C’s” of the world as citizens of society who need to be cared for with dignity and respect, not as Delta Platinum.

This blog is a part of the “Dialogues in Health Equity” series by the Health Equity Faculty Interest Group. They are committed to decreasing health disparities experienced by local and global communities by promoting social justice and health equity through nursing practice, research, education, and service.
Read more:
ABOUT THE AUTHORS

Kelley Robinson, MSN, CNM, is a PhD candidate at Johns Hopkins School of Nursing. She served as a full-time certified nurse midwife for 15 years, and at Johns Hopkins, has served as a clinical instructor for courses including Public Health Nursing and Nursing the Childbearing Family. She has extensive experience in maternal/newborn care under both normal and higher-risk conditions, and her PhD research examines the associations between housing instability experienced by pregnant women and maternal morbidities. Kelley earned her MSN at Yale School of Nursing.Mobile Health Clinics: Bringing Nursing to Those Experiencing Homelessness

Derek Lee, MSN, M.Eng a graduate of the MSN (Entry into Nursing) program, recipient of the Johns Hopkins Nurses’ Alumni Award, and is currently a DNP Family Primary Care NP student at the Johns Hopkins School of Nursing. His experience as a pharmaceutical bioengineer in addition to his current work in the emergency department has led to research interests in burnout, workplace violence, and reducing polypharmacy in the elderly.

Tiara D. Askew, MHS, MSN, is a recent graduate of the MSN (Entry into Nursing) program and recipient of the Research Award. She was a member of the Black Student Nurses Association and a Research Assistant for the Health Equity Faculty Interest Group. Her interests include cardiovascular health disparities and advancing health equity in clinical practice.